Sterilization Equipment: Essential Tools for Ensuring Laboratory and Clinical Safety
Sterilization is a cornerstone of safety in both laboratories and healthcare facilities. Without proper sterilization, harmful microorganisms such as bacteria, viruses, and fungi can survive on instruments, surfaces, and materials, creating risks of infection, contamination, and inaccurate experimental results. To prevent this, specialized sterilization equipment is used to completely eliminate or inactivate microorganisms.
Why Sterilization Matters

Main Types of Sterilization Equipment

Autoclaves (Steam Sterilizers)
- How it works: Uses high-pressure saturated steam (121–134°C) to kill microorganisms.
- Applications: Surgical tools, laboratory glassware, microbiological media, textiles.
- Advantages: Reliable, efficient, cost-effective.
- Limitations: Not suitable for heat-sensitive materials like plastics or electronics.

Dry Heat Sterilizers
(Hot Air Ovens)

Gas Sterilizers (Ethylene Oxide, ETO)
What They Are
Gas sterilizers, commonly using Ethylene Oxide (ETO), are specialized devices designed to sterilize heat- and moisture-sensitive medical equipment and laboratory materials. Unlike steam autoclaves or dry heat ovens, ETO sterilizers use a chemical gas that penetrates packaging and complex surfaces to inactivate microorganisms, including bacteria, viruses, fungi, and spores.
How They Work
1
2
3
4
Advantages
Effective for heat-sensitive and moisture-sensitive items.
Penetrates complex and sealed packaging, ensuring sterility of wrapped instruments.
Can sterilize electronics and plastics without damage.
Limitations
Toxicity: Ethylene oxide is hazardous; strict handling and ventilation are required.
Time-consuming: Aeration can take many hours, slowing turnaround.
Cost: Equipment and safety infrastructure are expensive.
Environmental regulations: ETO emissions must be carefully controlled.
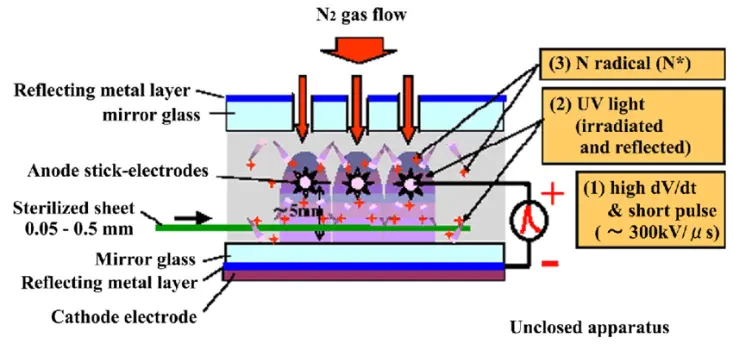
Plasma Sterilizers (Hydrogen Peroxide Plasma)
How it works: Generates plasma from hydrogen peroxide vapor to destroy microorganisms.
Applications: Endoscopes, surgical instruments, heat-sensitive devices.
Advantages: Fast cycles, safe by-products (water and oxygen).
Limitations: Limited penetration, not suitable for cellulose-based items.
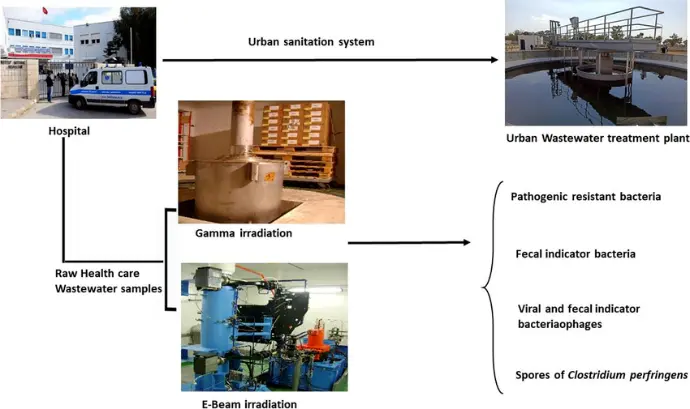
Radiation Sterilizers (Gamma & Electron Beam)
How it works: Uses ionizing radiation to destroy DNA of microorganisms.
Applications: Single-use medical devices, pharmaceuticals, food packaging.
Advantages: Ideal for large-scale industrial sterilization.
Limitations: High setup cost, requires specialized facilities.
Choosing the Right Sterilization Equipment
Selection depends on:
Type of material (heat-sensitive vs. heat-resistant).